Cervical cancer silently strikes millions of women worldwide. In the realm of women’s health, it demands our attention, awareness, and proactive measures. As per WHO, it is the fourth most common cancer type affecting women globally. There have been approximately 604000 new cases and 342000 deaths in 20201.
This blog aims to unravel the questions surrounding cervical cancer, shedding light on its causes and symptoms, and exploring a groundbreaking shield – the cervical cancer vaccine.
Armed with knowledge, we have the power to protect ourselves and our loved ones. Discovering the roots of cervical cancer and recognizing its early warning signs promote proactive health management.
Let’s unravel the layers of this critical health issue, paving the way for a world where cervical cancer is preventable.
Table of Contents
What is Cervical Cancer?
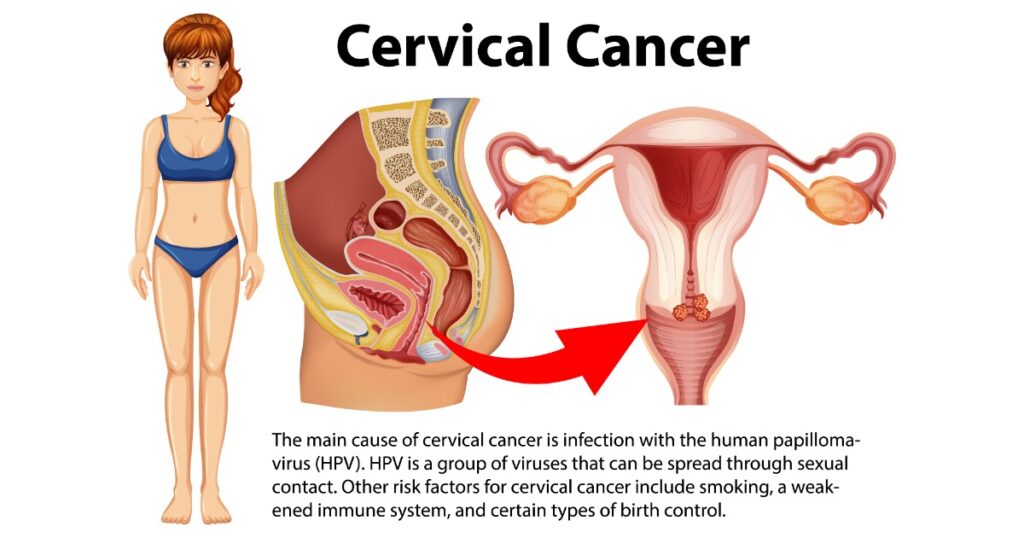
A type of cancer that begins in the cervix, the lower part of the uterus (womb) that connects to the vagina.
It primarily develops due to the uncontrolled growth of cells in the cervix, often triggered by persistent infection with high-risk strains of the human papillomavirus (HPV). HPV is a common sexually transmitted infection, and some can lead to cervical cancer if left untreated2.
The cervix plays a crucial role in a woman’s reproductive system. During childbirth, it dilates to allow the passage of the baby from the uterus to the vagina.
Unfortunately, this part of the reproductive system is susceptible to abnormal cell changes that may progress to cancer if not detected and treated in the early stages.
Notably, cervical cancer is highly preventable and, when detected early, is often curable. Regular screenings, such as Pap smears and HPV tests, are crucial for early detection, allowing healthcare professionals to identify and treat abnormal cell changes before they evolve into cancer.
Cervical Cancer Stages
Cervical cancer is staged to determine the extent of its spread and help guide treatment decisions. The staging system typically used for cervical cancer is the International Federation of Gynecology and Obstetrics (FIGO) staging system. It classifies cervical cancer into stages ranging from 0 to IV, with subcategories indicating the degree of tumour involvement.
Here is an overview of the different stages:
- Stage 0 (Carcinoma in situ): Also known as pre-cancer or carcinoma in situ. The abnormal cells are confined to the surface layer of the cervix and not present in deeper tissues. This stage is highly treatable, often with procedures like biopsy or laser surgery.
- Stage I: The cancer is confined to the cervix.
- Stage II: The cancer has spread beyond the cervix but is still within the pelvic area. There may be involvement of the upper two-thirds of the vagina but not the lower third.
- Stage III: The cancer extends to the pelvic sidewall and/or involves the lower third of the vagina.
- Stage IVA: The cancer has spread to adjacent organs beyond the pelvis, such as the bladder or rectum.
- Stage IVB: The cancer has spread to distant organs or regions, such as the lungs, liver, or bones.
Staging is determined through a combination of clinical examination, imaging studies, and sometimes surgical exploration. The stage of cervical cancer plays a crucial role in determining the appropriate treatment approach, which may include surgery, radiation therapy, chemotherapy, or a combination of these.
Cervical Cancer Symptoms
Cervical cancer may not always present noticeable symptoms in its early stages. However, as the disease progresses, person may exhibit various symptoms.
Here are some common symptoms of cervical cancer:
- Abnormal Vaginal Bleeding: Unusual bleeding between periods, after menopause, or during sexual intercourse can be a warning sign.
- Pelvic Pain: Persistent pelvic pain or discomfort, especially during sexual intercourse or a pelvic exam, may indicate the presence of cancer.
- Unusual Vaginal Discharge: Changes in the colour, consistency, or odour of vaginal discharge may occur. This may include increased discharge that may contain blood.
- Pain During Urination: Cervical cancer, when it spreads to nearby tissues, may cause discomfort or pain during urination.
- Back Pain or Leg Swelling: If the cancer has advanced and affects nearby organs, it may lead to back pain or swelling in the legs.
- Fatigue and Weight Loss: Advanced cancer stage can cause symptoms like fatigue and unexplained weight loss.
- Changes in Bowel Habits: In rare cases where cancer spreads to the rectum, it may cause changes in bowel habits or blood in the stool.
It’s crucial to note that these symptoms can also be associated with various non-cancerous conditions. However, if any of these signs persist or if you experience a combination of them, it’s essential to consult a healthcare professional for a thorough evaluation.
Cervical Cancer Causes
Cervical cancer is primarily caused by high-risk strains of the human papillomavirus (HPV). HPV is a group of viruses that can be transmitted through sexual contact. While HPV infection is the leading cause, there are also several cervical cancer risk factors:
- Human Papillomavirus (HPV) Infection: Persistent infection with certain high-risk strains of HPV is the primary cause of cervical cancer. HPV types 16 and 18 are particularly linked to a higher risk of developing this cancer. HPV is a common sexually transmitted infection, and most sexually active individuals will be exposed to it at some point.
- Lack of HPV Vaccination: The HPV vaccine is a highly effective preventive measure against cervical cancer. Vaccination is recommended for both boys and girls before they become sexually active to provide immunity against the most common high-risk HPV strains.
- Weakened Immune System: Individuals with weakened immune systems due to conditions such as HIV/AIDS or immunosuppressive medications have an increased risk of developing cervical cancer.
- Cigarette Smoking: Smoking has been identified as a risk factor for cervical cancer. It makes a person more susceptible to HPV infection and increases the risk of cancer development.
- Long-Term Use of Birth Control Pills:Women who have used birth control pills for an extended period may have a slightly increased risk of cervical cancer.
- Having Many Sexual Partners: Engaging in sexual activity with multiple partners or having a partner with a history of multiple sexual partners increases the likelihood of exposure to HPV, thereby elevating the risk of cervical cancer.
- Early Onset of Sexual Activity: Initiating sexual activity at an early age may increase the risk of HPV infection.
Understanding these risk factors is crucial for prevention and early detection.
Cervical Cancer Treatment

Cervical cancer treatment is tailored to the specific stage of the cancer, the patient’s overall health, and individual preferences. The primary treatment modalities include surgery, radiation therapy, and chemotherapy. In some cases, a combination of these approaches may be recommended. Here’s an overview of the main treatment options:
- Surgery: In cases of early-stage cervical cancer (Stage 0 or IA), where the cancer is confined to the surface layer of the cervix, a cone biopsy or conization may be performed. This involves removing a cone-shaped piece of tissue containing the abnormal cells.
- Radiation Therapy: Radioactive sources are placed directly inside or near the tumour, delivering a high dose of radiation to the cancer while minimizing exposure to surrounding healthy tissues.
- Chemotherapy: Drugs that target and kill rapidly dividing cells, including cancer cells, are administered intravenously or orally. Chemotherapy may be used in combination with radiation therapy (chemoradiation) to enhance treatment effectiveness.
- Immunotherapy: Immunotherapy is a treatment that stimulates the body’s immune system to recognize and attack cancer cells.
- Hysterectomy: In more advanced cases or when the cancer has not responded to other treatments, a hysterectomy may be recommended. This involves the removal of the uterus and, in some cases, surrounding tissues such as the cervix, upper vagina, and nearby lymph nodes.
The choice of treatment depends on factors such as the stage of the cancer, the patient’s overall health, and individual circumstances.
Individuals diagnosed with cervical cancer need to work closely with a multidisciplinary healthcare team, including gynaecologists and medical oncologists, to develop a personalized treatment plan.
Regular follow-up care is also crucial to monitor for any signs of recurrence or potential long-term side effects of treatment.
Cervical Cancer Vaccine

The cervical cancer vaccine refers to vaccines designed to prevent infection with high-risk strains of the human papillomavirus (HPV), which is the primary cause of cervical cancer.
The vaccines target specific HPV types that are known to be associated with an increased risk of cervical cancer, as well as other HPV-related cancers and diseases. The two main vaccines currently available are Gardasil 9 and Cervarix.
- Gardasil 9: Gardasil 9 is a vaccine that protects against nine different types of HPV. It provides immunity against the most common high-risk HPV strains (16 and 18) associated with cervical cancer, as well as strains 31, 33, 45, 52, and 58. Additionally, it includes protection against low-risk HPV types 6 and 11, which are responsible for the majority of genital warts.
- Cervarix: Cervarix primarily targets HPV types 16 and 18, the two most common high-risk strains associated with cervical cancer.
How the Vaccines Work
These vaccines work by stimulating the immune system to produce antibodies against specific HPV types. If a person is later exposed to those HPV types through sexual activity, the immune system recognizes and fights the virus, preventing infection and the potential development of cervical cancer.
Administration
The vaccines are typically administered in a series of two or three doses, depending on the age of the individual at the time of the first dose. The recommended age for vaccination is usually between 9 and 26 years, ideally before the onset of sexual activity and potential exposure to HPV.
Effectiveness
Clinical trials have demonstrated that both Gardasil 9 and Cervarix are highly effective in preventing targeted HPV infections and associated cancers. They have been shown to significantly reduce the incidence of cervical precancers, providing long-lasting protection.
Additional Benefits
In addition to preventing cervical cancer, these vaccines also protect against other HPV-related cancers, including vulvar, vaginal, anal, and oropharyngeal cancers. The vaccines contribute to the reduction of genital warts caused by low-risk HPV types.
Safety
The vaccines have been extensively studied and are generally considered safe. Common side effects include pain at the injection site, fever, and mild reactions. Severe adverse reactions are rare.
Impact on Public Health
The introduction of HPV vaccines has the potential to significantly reduce the incidence of cervical cancer globally, contributing to public health efforts to eliminate this preventable cancer.
Individuals, parents, and healthcare providers need to discuss and consider HPV vaccination as a crucial preventive measure against cervical cancer and other HPV-related diseases.
Cervical Cancer Vaccine Price in India
The vaccine can be obtained as part of a government-sponsored vaccination program. However, it generally ranges between Rs. 2000-4000 privately.
Frequently Asked Questions
What are some stage 1 cervical cancer symptoms?
In Stage 1, symptoms may include abnormal vaginal bleeding between periods, after intercourse, or postmenopausal bleeding. Some individuals may also experience mild pelvic pain or discomfort, pain during sexual intercourse, and changes in vaginal discharge.
What causes cervical cancer besides HPV?
Besides HPV, additional risk factors include weak immune health, cigarette smoking, early onset of sexual activity, long-term use of birth control pills, and multiple sexual partners.
What is the cervical cancer survival rate?
The survival rate may vary based on several factors, including the stage at diagnosis, the extent of spread, age, overall health, and the effectiveness of the treatment. According to the American Cancer Society, the overall five-year survival rate for all stages combined is around 66%.
What are the visible signs of cervical cancer?
Common signs may include abnormal vaginal bleeding, pelvic pain, pain during sexual intercourse, fatigue, weight loss, and swelling in the legs.
Can cervical cancer be cured?
It can be treated and, in some cases, cured, especially when detected at an early stage. It is important to note that individual responses to treatment can vary, and successful outcomes depend on factors such as the cancer’s characteristics and how well it responds to the treatment.
Sources
- World Health Organization: WHO. (2023, November 17). Cervical cancer. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer ↩︎
- What is cervical cancer? (2023, June 15). National Cancer Institute. https://www.cancer.gov/types/cervical ↩︎

A very informative and awareness spreading blog…. 👍